April 7th, 2021 • Sharon Dolovich and Poornima Rajeshwar
SARS-CoV-2 Variants go to Prison: What Now?
It was only a matter of time.
In September, public health officials in the United Kingdom reported the local emergence of B.1.1.7, a new, more contagious variant of SARS-CoV-2. By mid-February, a correctional officer at the Michigan Department of Corrections’ (MDOC) Bellamy Creek Correctional Facility tested positive for the variant, marking B.1.1.7’s first appearance in an American prison. Over a month later, at least 420 prisoners across three Michigan state facilities have been found to have the variant, which now accounts for nearly 40% of confirmed B.1.1.7 cases among the Michigan population overall.
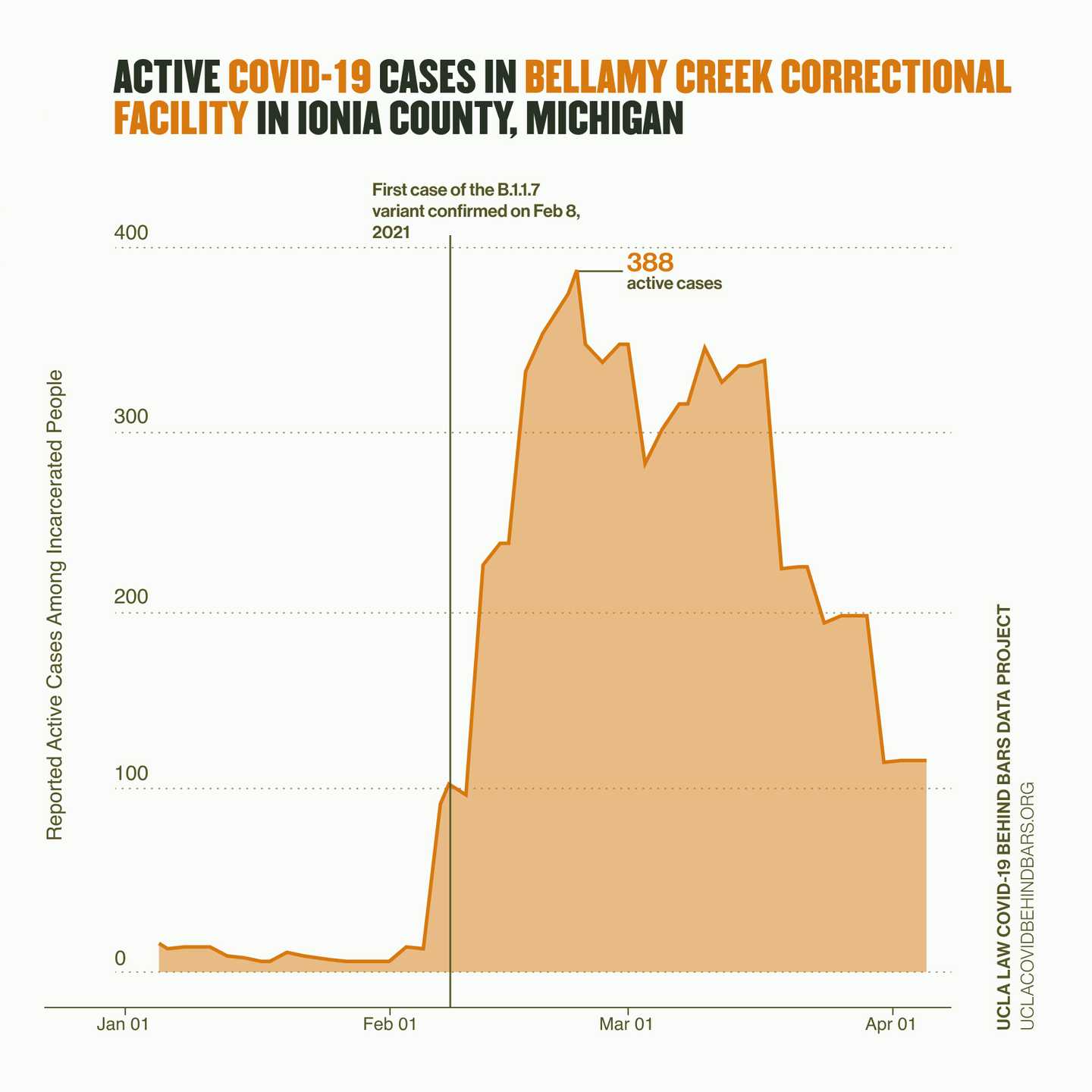
Figure: After a correctional officer tested positive with B.1.1.7 at Bellamy Creek in February, MDOC has been conducting daily rapid antigen tests for all incarcerated people and staff under an emergency public health order issued by the state health department. According to the public information officer at MDOC, the sustained outbreak can be attributed partly to B.1.1.7 and partly to the new testing regime, which, having changed from weekly to daily tests, resulted in the detection of more cases.
MDOC is not the only correctional system dealing with variants. B.1.1.7 has been found in a Maryland prison, and by mid-March, eight people at Buena Vista Correctional facility in Colorado, including two staff members, tested positive for B.1.351, the variant first detected in South Africa and that is believed to spread more easily. Though MDOC is the only jurisdiction so far to report a prison outbreak led by a new variant, most other prison systems lack the methods of epidemiological tracking through genomic surveillance which is critical to detecting variants. With B.1.1.7 constituting 27% of new cases in the general population across the country, and now present in all 50 states and the District of Columbia, it is vital that carceral institutions closely monitor for new variants.
A more contagious virus could prove catastrophic behind bars. As we’ve seen over the past year, COVID-19 spreads alarmingly fast in carceral facilities, where people live packed together and social distancing is often impossible. Adequate PPE is not always available and not scrupulously used where present. Systemwide ventilation is poor. People are lucky to have soap and warm water, let alone hand sanitizer. And, multiple times a day, staff and incarcerated workers still move through every corner of every facility, delivering food and medical care—and the virus.
In July, one of us (Dolovich) co-authored, along with Brendan Salonar and Julie Ward of Johns Hopkins Bloomberg School of Public Health and Grace DiLaura and Kalind Parish of our UCLA Data Project, a paper in JAMA reporting that people living in state and federal prisons experienced COVID-19 infection at 5.5 times the rate of the general public, with an age-adjusted death rate 3 times higher.
In a more recent study published in the American Journal of Preventive Medicine, the same team demonstrated that the incarcerated are not the only ones at elevated risk: prison staff infection rates are more than 3 times that of the population as a whole.
As B.1.1.7 and other highly contagious strains circulate, the health of prison staff and residents continues to be in jeopardy. With COVID-19 cases once again on the rise in the U.S., and several prison systems re-opening visitation, containing viral spread must remain a priority.
There remains time to act, but the window is closing fast. Since the pandemic began, advocates, including health experts, have been calling for releases to allow for those left inside to social distance. In February, recognizing the dangers that COVID-19 still presents, the North Carolina prison system agreed to release more than 3,500 people from state facilities. This is a sensible public health measure that should serve as a model to other prison systems.
Even short of that critical response, however, options remain.
Mass testing is an essential first step. Because outbreaks explode so quickly behind bars, it is imperative to conduct regular mass testing of everyone inside, not just those exhibiting symptoms. Further, there needs to be concerted effort to regularly monitor for virus mutations through genomic surveillance.
But as on the outside, the ultimate goal in prisons is herd immunity through vaccination. The new variants are now being studied for their resistance to vaccines, but corrections officials need to get ahead of this problem and get everyone immunized as soon as possible before more contagious mutations emerge. To date, all state prison systems and the Federal Bureau of Prisons are vaccinating staff. Though most of these systems have offered the vaccine to some prisoners, the share of the incarcerated population eligible to receive the vaccine varies widely, with some states such as Florida—which has not vaccinated a single incarcerated person—putting elderly or medically vulnerable prisoners behind their free-world counterparts.
Even when the vaccine has been offered, acceptance rates among prisoners vary widely—as high as 75% in Rhode Island and Indiana prisons and as low as 30% in some Massachusetts jails. On the staff side, several states such as Massachusetts and North Carolina report acceptance rates of 50% and lower, with states like Illinois registering vaccine uptake among staff as low as 27%.
To counter vaccine hesitancy, corrections agencies must develop a strategy for vaccine education. Several readily available resources, including AMEND’s FAQs on vaccines and the guide we published in Prison Legal News, offer clear and accessible information about the vaccine as a way to increase confidence and decrease suspicion among incarcerated people. Where refusal rates are high, creativity and flexibility may also be necessary. Virginia, seeking to increase vaccine uptake, has offered prisoners care packages and email and phone credits. In North Carolina and Delaware, incentives include modest sentence reductions and commissary benefits.
Prison officials should also act to engender confidence in the vaccine itself—perhaps by getting their own vaccines in full view of prison residents. During the swine flu outbreak of 2009, the associate warden at Rikers Island did just this, and it proved highly effective.
The nation’s prisons and jails are full of people—prisoners and staff—who lack the means to protect themselves. They are already getting infected and dying of COVID-19 at much higher rates than the public as a whole, and with B.1.1.7 and other more contagious variants in circulation, the danger will only grow. Regular mass testing and effective quarantine should be immediately and universally adopted. And now that we finally have a powerful defense—the vaccine—we need to get it into prisons as rapidly and efficiently as possible.
Data visualization by Erika Tyagi.
next post
April 15th, 2021 • Poornima Rajeshwar and Erika Tyagi
Vaccine Hesitancy Behind Bars: Causes and Concerns
A new MMWR study finds that distrust of correctional institutions and lack of information are leading causes for COVID-19 vaccine hesitancy among incarcerated people. Correctional agencies must take crucial steps to inspire confidence in the vaccine and encourage uptake of this life-saving inoculation.